Table of contents :
- Introduction.
- Risk factor.
- Pathology.
- Signs and symptoms.
- Diagnostic criteria for PCOS.
- Lab investigation.
- PCOS Relationship with infertility.
- Management
1)Introduction: PCOS polycystic ovarian syndrome/ disorder.
Also known as Stein levelthal syndrome. It’s the most common endocrine and metabolic syndrome in females. Its incidence is 10%.
3 main components of PCOS :
- Increase androgen levels
- Ovulatory dysfunction
- Polycystic Ovaries
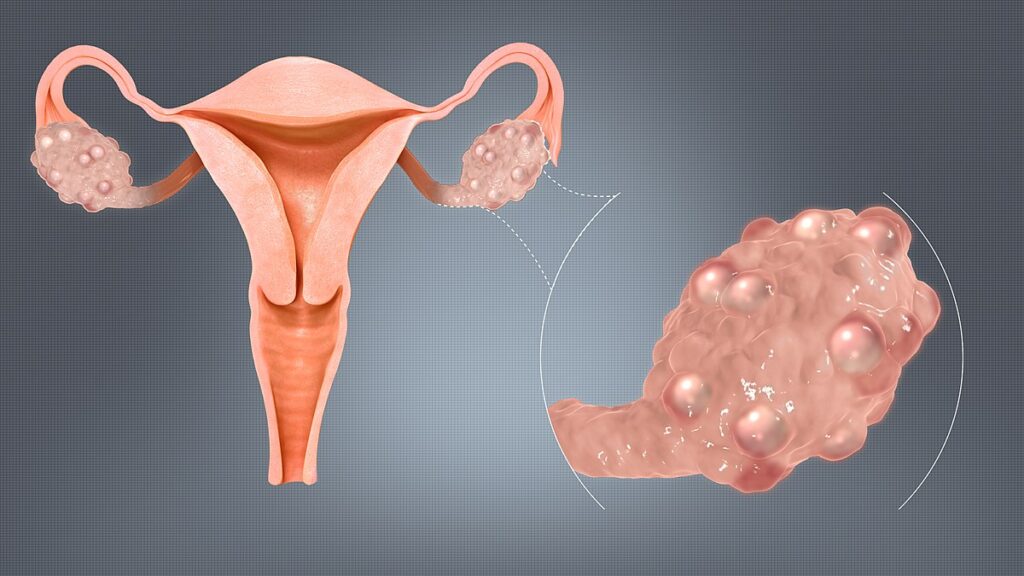
PCOS (polycystic ovarian syndrome) means it means cyst formation inside the ovaries. These cysts are the unruptured follicles in the ovaries..
Women with PCOS may experience irregular menstrual cycles, anovulation (lack of ovulation), and may develop multiple small cysts on their ovaries visible on ultrasound.
2) Risk factor for developing PCOS:
- Obesity
- Insulin resistance
- Type 1,2 diabetes mellitus
- Women with history of premature adrenarche
- Ethnicity: Mexican, Australian and south asian
- Genetics: h/o ist degree relative with PCOS.
- Some drugs like anti epileptic drugs eg valproic acid.
3) Pathology:
Main etiology is an increase in the androgen production by the ovaries .
- Increase in androgen
- Folliculotoxic effect.
- Multiple small follicles with arrested growth
- No dominant follicles.
- No ovulation.
The main pathological site is ovaries. Androgen levels increase because of the ovaries not because of the adrenals.
4) Signs and symptoms :
Signs:
Signs of Excess Androgens (Male Hormones)
Hirsutism – excessive hair growth on the face, chest, abdomen, or thighs
Acne – especially on the face, chest, and upper back
Hair thinning or male-pattern baldness
⚖️ Metabolic Changes
Weight gain or difficulty losing weight
Insulin resistance (can lead to prediabetes or type 2 diabetes)
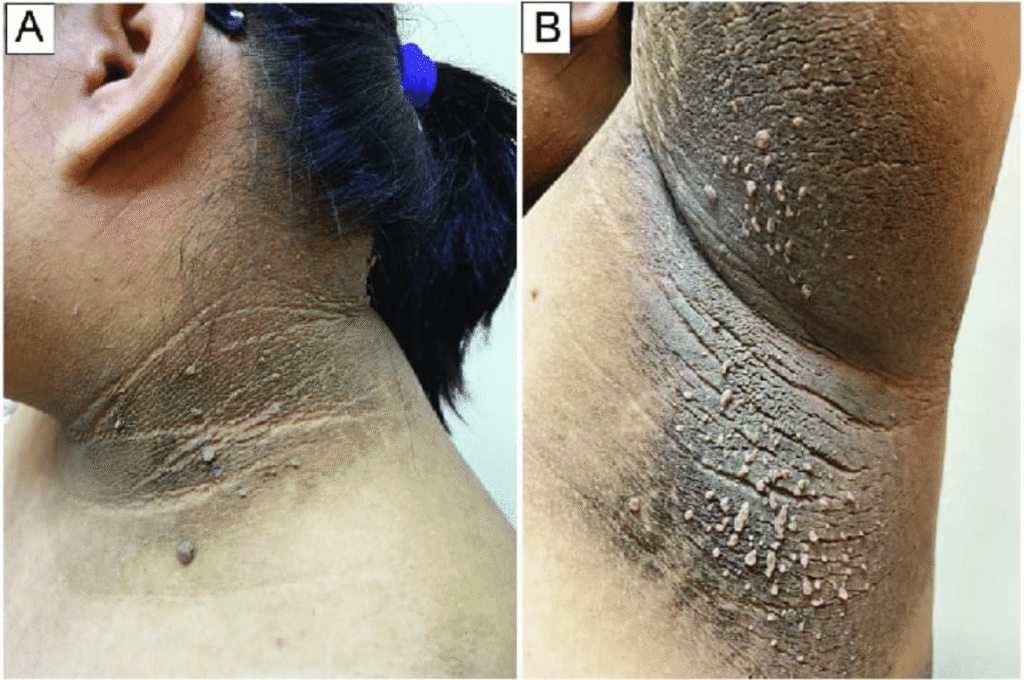
Darkening of skin (acanthosis nigricans) around the neck, armpits, or groin
Increased cholesterol or triglyceride levels
🩸 Reproductive Symptoms
Infertility or difficulty conceiving due to irregular ovulation
Polycystic ovaries seen on ultrasound – multiple small cysts (immature follicles)
🧠 Other Possible Signs
Mood changes, anxiety, or depression
Fatigue or low energy
Sleep problems, such as sleep apnea (especially if overweight)
Symptoms :
1. Menstrual Problems like Irregular or missed periods (most common symptom)Heavy bleeding during periods , Fewer than 8 periods a year or long gaps between cycles.
2.Excess facial or body hair (hirsutism) — on the chin, chest, or abdomen.
3.Severe acne — especially on the face, chest, or upper back.
4.Hair thinning or male-pattern baldness.
5. Weight and Metabolic Changes like Weight gain (especially around the abdomen)
Difficulty losing weight , Dark, velvety skin patches (acanthosis nigricans), usually on the neck, armpits, or groin. Insulin resistance or high blood sugar.
6. Reproductive Symptoms like Difficulty conceiving due to lack of regular ovulation
7. Emotional and Other Symptoms likeMood swings, anxiety, or depression
Fatigue or low energy, Sleep problems (like sleep apnea, especially in overweight women).
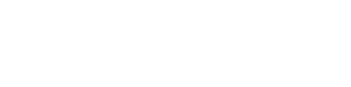
5) Diagnostic criteria for PCOS:
NAME OF CRITERIA IS : ROTTERDAM CRITERIA
Any 2 of the following 3 should be present to make a provisional diagnosis of PCOS:
- INCREASE ANDROGEN LEVELS: On biochemistry hyperandrogenaemia or
as hirsutism : hyperandrogenism.
- OVULATORY DYSFUNCTION: As oligomenorrhea/ amenorrhea
- ON USG: 1 OR both ovaries: >12 follicles;2-9mm in size (<1cm ). Volume of ovary >10cc.
6) lab investigation:
Here are the key laboratory investigations recommended (or discussed) in Williams’ Gynecology / Williams’ textbooks:
Basic & First-Line Labs
These help confirm the presence of PCOS (by showing hormonal imbalance) and also rule out other causes.
1)Serum total testosterone : To document hyperandrogenemia (biochemical hyperandrogenism) In PCOS, mild to moderately elevated levels; very high levels prompt evaluation for androgen-secreting tumors.
2)Free testosterone / free androgen index / SHBG (Sex Hormone Binding Globulin):To assess biologically active (free) androgen.SHBG is often low in PCOS (due to insulin resistance), raising free testosterone fraction.
3)DHEA-S (Dehydroepiandrosterone sulfate) To evaluate adrenal source of androgens Modestly elevated in PCOS; markedly high suggests adrenal pathology.
4)17-hydroxyprogesterone (17-OHP): To exclude late onset congenital adrenal hyperplasia (CAH) If elevated (especially in the follicular phase), CAH has to be excluded.
5)LH and FSH (luteinizing hormone / follicle-stimulating hormone) : To detect the typical “LH:FSH > 2:1 or > 3:1” pattern (though not universally present) In PCOS, LH may be moderately elevated relative to FSH. But normal LH/FSH does not exclude PCOS.
6)Prolactin : To rule out hyperprolactinemia which can cause menstrual abnormalities Elevated prolactin must be ruled out as differential.
7)TSH / Free T4: To exclude thyroid dysfunction as a cause of menstrual irregularity Hypothyroidism or hyperthyroidism can mimic or contribute to menstrual problems.
8)Fasting glucose / 2-hour oral glucose tolerance test (OGTT):To assess for insulin resistance / glucose intolerance / diabetes risk Many PCOS patients have insulin resistance; 2-h OGTT is more sensitive.
9)Fasting insulin / HOMA-IR To quantify insulin resistance Optional, depending on resources and clinical suspicion.
10)Lipid profile (cholesterol, triglycerides, HDL, LDL):To check for dyslipidemia (common metabolic comorbidity)
Optional / Specialized / Provocative Tests (Advanced):
These are not always done routinely but may help in research settings or in borderline / difficult cases.
1)GnRH agonist (GnRHag) stimulation test — to assess ovarian hyperandrogenism more directly.
2)hCG stimulation test — similarly to assess androgen response of the ovary.
3)Dexamethasone suppression test (diurnal androgen suppression test, DAST) — to determine adrenal contribution to androgen levels.
4)Other adrenal function tests (e.g. ACTH stimulation) if adrenal source of androgen excess is suspected.
PCOS is a diagnosis of exclusion — before diagnosing PCOS, other endocrine conditions like CAH, Cushing syndrome, androgen-secreting tumors, hyperprolactinemia, thyroid disease must be excluded. Hormone measurements should be done in the early follicular phase (if the patient has menses) or during a time when the hormonal milieu is more stable
7)PCOS Relationship with infertility:
1. Ovulatory Dysfunction (Main Cause):
In PCOS, hormonal imbalance — especially increased LH, androgens, and insulin resistance — disrupts normal ovulation.
Instead of one dominant follicle maturing and releasing an egg, multiple small follicles (cysts) form and remain arrested.
This leads to anovulation (no ovulation) or oligo-ovulation (infrequent ovulation) → no egg available for fertilization → infertility.
2. Hormonal Imbalance
↑ LH/FSH ratio (usually >2:1)
↑ Androgens (testosterone, androstenedione)
↑ Insulin (insulin resistance)
↓ Progesterone (due to lack of corpus luteum after anovulation)
These changes interfere with follicular maturation and endometrial receptivity.
3. Endometrial Dysfunction
Without regular ovulation, progesterone is not secreted, causing unopposed estrogen exposure.
Endometrium becomes thick and irregular, reducing its receptivity for implantation.This may lead to infertility or early pregnancy loss.
4. Insulin Resistance and Obesity
Many PCOS women have insulin resistance, which increases androgen production by the ovaries.Obesity worsens hormonal imbalance and anovulation.Weight reduction often helps restore ovulation and fertility.
5. Other Factors
Altered GnRH pulse frequency → increased LH secretion.
Impaired follicular maturation → poor oocyte quality.
Management:
Ist line management: lifestyle modification.
Even 5 % weight reduction can lead to ovulatory cycles. Recommended in overweight + obese PCOS females. Advise hypocaloric diet + brisk walking and exercise. Weight loss improves insulin resistance , increases sex hormone binding globulin that results in decreased androgen level.
DOC for PCOS: in general, it is oral contraceptive pills. This is for menstrual irregularities, ocp’s given for : 3 weeks on and 1 week off. Total duration of treatment with ocp’s 6month
4th generation ocp’s: DROSPIRINONE , CYPROTERONE.
Ocp’s are started at day 1 OR within 5 days of cycles.
Progesterone reduces endogenous LH which acts on theca cells to produce androgen. Hence hirsutism is treated.
As natural estrogen is reduced by ocp’s, it leads to thinning of the endometrium. So endometrial hyperplasia is prevented.
Alternative for ocp’s ( ocp’s contraindicated):
Every 1 to 3 months ( when they don’t menstruate ) : give progesterone withdrawal.
Medroxy progesterone acetate: given 5 to 10mg daily orally for 12 days, this leads to menstruation. It doesn’t act as a contraceptive and doesn’t help in reducing acne and hirsutism.
DOC for insulin resistance: metformin ( 500mg TDS with meals)
Indications: 1) PCOS with impaired glucose tolerance.
2) increase fasting insulin.
3) Acanthosis nigricans.
4) family history of diabetes mellitus.
Management of infertility:
In PCOS infertility is because of anovulation, and even if they ovulate, egg quality is poor and low endometrial receptivity.
Ist line drugs :
DOC : LETROZOLE.
2ND LINE : CLOMIPHINE CITRATE.
These drugs cause growth of follicles
2nd line drugs: HMG (75 UNITS OF LH AND FSH).OR LAPAROSCOPIC OVARIAN DRILLING.
3rd line :
Pulsatile GnRh.
IVF.
PCOS :